At five months old, my son was diagnosed with infantile spasms (IS)—a rare, catastrophic form of epilepsy. Before his diagnosis, his unusual movements were mistaken for startle reflexes, and his frequent crying was thought to be colic. But deep down, we knew something wasn’t right.
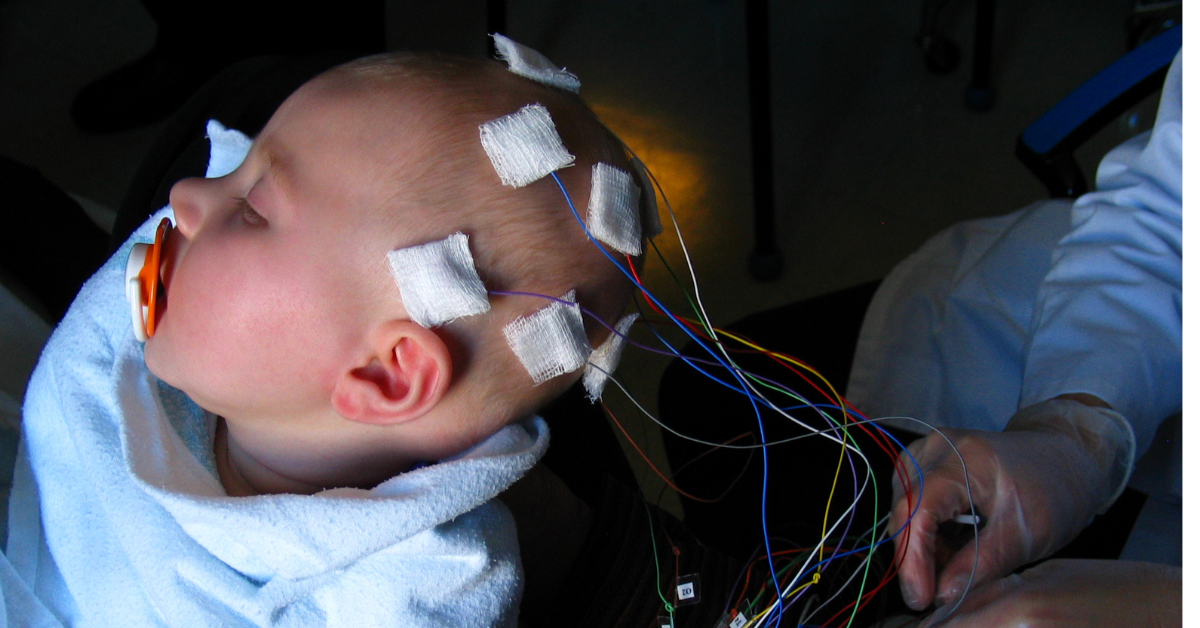
An overnight EEG confirmed our fears, and his neurologist started frontline treatments: ACTH and vigabatrin. They worked briefly, but the seizures returned. For two years, he endured daily seizures despite trying countless medications. It was devastating.
The cause of his seizures was a stroke before birth, making it unlikely that medication alone could help. When he was two years old, we found hope: he underwent a functional hemispherectomy, a surgery to disconnect one side of his brain. It was the hardest decision of our lives, but the moment the surgery was done, his seizures stopped. He began to grow, learn, and thrive.
Today, at 21, my son lives in an apartment, works at a theater, takes college classes, and has a happy, fulfilling life. He still has challenges, but he is living proof that early and aggressive treatment for IS, including surgery, can change everything.
If you’re here, you may feel scared or overwhelmed. Here’s what you need to know about IS and surgical options based on the latest research and expert insights.
What Are Infantile Spasms?
Infantile spasms are a severe type of epilepsy that typically begins in the first year of life. They often appear as subtle movements like head nods, body jerks, or brief stiffening episodes. While these movements might seem minor, these seizures can cause serious damage to a baby’s development if not treated quickly.
Infantile spasms are a neurological emergency.
Time is critical because early diagnosis and treatment offer the best chance of stopping seizures and protecting your child’s brain.
Why Surgery is Needed
According to Dr. Shaun Hussain, Director of the Infantile Spasms Program at UCLA, infantile spasms are the most severe form of epilepsy in children under age one. For some children, medications stop the spasms. But if medications fail to control spasms—and they do in about 80% of cases—surgery may be needed.
Dr. Aria Fallah, Director of Pediatric Neurosurgery at UCLA, explains that surgery can stop seizures and help children thrive—especially when their seizures are caused by specific brain issues like cortical dysplasia or stroke. Surgery isn’t right for every child, but for those who qualify, it can be life-changing.
Types of Surgery for IS:
- Resective Surgery: Removes or disconnects the part of the brain causing seizures. This is the most effective option for children with focal brain abnormalities. Hemispherectomy (removal or disconnection of one hemisphere of the brain) has shown positive outcomes in carefully selected patients.
- Corpus Callosotomy: Severs the connection between the brain’s two halves to prevent seizures from spreading. While not a cure, it can help make some children candidates for resective surgery.
- Vagus Nerve Stimulation (VNS): A device that sends electrical signals to the brain. While less effective for IS, it may be considered for children who are not candidates for other surgeries.
What Does the Research Say?
- Surgery Can Save Lives – Early studies, like Treatment of Infantile Spasms: Medical or Surgical? (Shields et al., 1992), highlighted that surgery is often the best option for children with drug-resistant IS caused by brain abnormalities.
- Act Fast – Delays in diagnosing and treating IS reduce the chances of a good developmental outcome (Pellock et al., 2010). Early surgery is especially critical for infants with structural causes of seizures.
- Specialized Care Matters – Subtle brain abnormalities, like cortical dysplasia, are often missed in general settings. According to Dr. Hussain, experienced epilepsy centers using advanced imaging can identify these lesions and recommend surgery promptly.
Time is brain.
What Should Parents Do?
- Trust your instincts – If your baby’s movements seem unusual, seek medical advice promptly. Infantile spasms are often mistaken for reflux or normal baby movements, but they are a medical emergency.
- Get the right care – Often, pediatricians and emergency department physicians are not familiar with infantile spasms. Overnight video EEG monitoring can provide more detailed information than a short EEG. Ask to meet with a neurologist who specializes in epilepsy, known as an epileptologist.
- Ask about surgery – If your child doesn’t respond to two medications, discuss surgical options with your doctor. Early intervention saves brain function and gives your child the best chance to thrive.
- Get a second opinion – If your child’s MRI appears normal, ask for a review at a level 4 epilepsy center. Subtle brain lesions can be missed.
Fear the Spasms, Not the Surgery
Infantile spasms are devastating, but there is hope. Epilepsy surgery gave my son a second chance—and your child deserves that chance, too.
Remember, the most dangerous thing is ongoing spasms. As Dr. Fallah said, “The risks of surgery are far outweighed by the risks of ongoing spasms.”
Every moment matters. Advocate fiercely, act quickly, and know that our community is here to support you.
Let’s work together to raise awareness of infantile spasms.
Resources and Support
You are not alone. Here are some helpful videos and webinars to guide you:
- Epilepsy Surgery for Infantile Spasms: This special webinar in our series “Let Talk About Epilepsy Surgery” introduces you to epilepsy surgery to stop infantile spasms. Monika Jones, Founder and Executive Director of the Pediatric Epilepsy Surgery Alliance, is joined by Dr. Aria Fallah, Director of the Pediatric Neurosurgery Program and Dr. Shaun Hussain, Director of the Infantile Spasms Program, both at Mattel Children’s Hospital (UCLA). They provide an overview of infantile spasms and the criteria for resection surgery, corpus callosotomy, and vagus nerve stimulation.
- Infantile Spasms Are An Emergency: This public service announcement was produced by Monika Jones, Founder and Executive Director of the Pediatric Epilepsy Surgery Alliance, on behalf of the Infantile Spasms Action Network as part of Infantile Spasms Awareness Week 2018 campaign. The video went viral and is still circulated widely today. It sends a clear and sober message to parents and clinical providers that infantile spasms should be considered a medical emergency, requiring immediate diagnosis and treatment. Learn how to recognize IS and the importance of early intervention.
- The Infantile Spasms Action Network (ISAN) is a collaborative network of 30+ national and international entities dedicated to raising awareness of infantile spasms (IS).
- The Pediatric Epilepsy Surgery Alliance’s website has a wealth of resources to help you understand your options, such as What is Pediatric Epilepsy Surgery?, Risks of Drug-Resistant Epilepsy, and much more. You can also connect with a parent who has been on this journey via our Parent Support Navigator Program.
Sources
Chen, S., et al. (2021). Timing of Surgical Intervention and Outcomes in Children with Drug-Resistant Infantile Spasms. Epilepsia, 62(6), 1345-1354.
Gettings JV, Shafi S, Boyd J, et al. The Epilepsy Surgery Experience in Children With Infantile Epileptic Spasms Syndrome at a Tertiary Care Center in Canada. Journal of Child Neurology. 2023 Mar;38(3-4):113-120. DOI: 10.1177/08830738231151993. PMID: 36788207.
Hernandez, M., et al. (2023). Advanced Imaging for Identifying Surgical Candidates in Drug-Resistant Infantile Spasms: A Systematic Review. Child Neurology Journal, 10(1), 12-25.
Kolosky T, Goldstein Shipper A, Sun K, Tozduman B, Bentzen S, Moosa AN, Erdemir G. Epilepsy surgery for children with epileptic spasms: A systematic review and meta-analysis with focus on predictors and outcomes. Epilepsia Open. 2024 Aug;9(4):1136-1147. doi:10.1002/epi4.13007
Pellock JM, Hrachovy R, Shinnar S, Baram TZ, Bettis D, Dlugos DJ, Gaillard WD, Gibson PA, Holmes GL, Nordl DR, O’Dell C, Shields WD, Trevathan E, Wheless JW. Infantile spasms: a U.S. consensus report. Epilepsia. 2010 Oct;51(10):2175-89. doi:10.1111/j.1528-1167.2010.02657.x
Shields WD, Shewmon DA, Chugani HT, Peacock WJ. Treatment of Infantile Spasms: Medical or Surgical? Epilepsia. 1992 Jul-Aug;33 Suppl 6:S35-40. doi:10.1111/j.1528-1157.1992.tb06224.x
Wu, T., et al. (2022). Focal Brain Surgery in Children with Infantile Spasms: A Review of Outcomes and Best Practices. Journal of Pediatric Neurosurgery, 15(3), 214-221.
about the author

Audrey Vernick is our Director of Patient and Family Advocacy. She is the parent of a child who had hemispherectomy for seizures caused by stroke. She holds a level 2 certification in Special Education Advocacy Training from the Council of Parent Attorneys and Advocates and is certified by The ARC in future planning. She also serves on the International League Against Epilepsy’s Social Work and Social Services Section.